Why Post-COVID Brain Fog Mimics Early Alzheimer's Disease
Last updated: October 2025
Many people recovering from COVID-19 are facing a new challenge—persistent brain fog. After the virus passes, symptoms like trouble focusing, forgetfulness, and feeling mentally “slow” can linger for months or even years. This condition, known as long-COVID brain fog, has striking similarities to early Alzheimer's disease, leading many to wonder if these post-COVID issues are related to cognitive decline. Recent research suggests that there is indeed an overlap between the two. Understanding this connection is crucial for finding effective treatment strategies.
What is Post-COVID Brain Fog?
Post-COVID brain fog is a condition where individuals experience cognitive difficulties long after recovering from the initial infection. Symptoms include:
- Memory issues, such as forgetting names or recent events
- Difficulty concentrating or staying focused
- Slower processing speed or feeling mentally “foggy”
- Difficulty finding the right words in conversation
While these symptoms seem harmless at first, they can worsen and resemble the early stages of Alzheimer’s. However, the causes of post-COVID brain fog are more complex than simple fatigue. Research has shown that the same mechanisms contributing to Alzheimer’s can also affect the brain after COVID-19 infection.
How Post-COVID Cognitive Decline Mimics Early Alzheimer's Disease
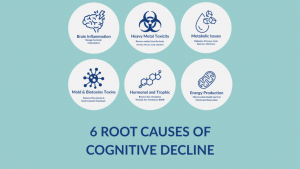
There are several shared factors between long-COVID brain fog and early Alzheimer’s. These include:
- Neuroinflammation: COVID-19 triggers an immune response that causes inflammation in the brain. This inflammation damages neurons and disrupts cognitive function, similar to what occurs in Alzheimer’s disease.
- Reduced Blood Flow: COVID-related microclots and vascular damage impair blood flow to the brain. This, in turn, reduces oxygen and nutrients reaching the brain’s most vital areas, including those responsible for memory and decision-making.
- Mitochondrial Dysfunction: Both Alzheimer’s disease and post-COVID cognitive decline can cause mitochondrial dysfunction, leading to reduced energy production in brain cells. This deprives neurons of the fuel needed to function properly.
- Hormonal Imbalances: Post-COVID patients often experience disruptions in cortisol, thyroid hormones, and sex hormones—imbalances that also accelerate cognitive decline in Alzheimer’s patients.
Each of these factors contributes to cognitive decline, causing the brain to function less efficiently and, in some cases, to shrink. Inflammation, poor circulation, and mitochondrial dysfunction are all processes that damage neurons, leading to symptoms that mimic the early signs of Alzheimer’s disease.
The ReCODE Program: A Solution for Post-COVID Cognitive Decline
At The Carroll Institute, we treat post-COVID cognitive decline with the same precision medicine approach that has successfully reversed Alzheimer’s disease—through the ReCODE Program. Unlike traditional treatments, which only manage symptoms, the ReCODE Program addresses the root causes of cognitive decline. It targets the factors that disrupt brain function and provides a personalized treatment plan that restores cognitive health.
Our program includes:
- Inflammation reduction: We identify and address inflammation triggers such as lingering viral particles, toxins, and immune dysfunction.
- Neuroplasticity exercises: Functional Neurology-based exercises stimulate brain regions that have been affected by inflammation, helping to rebuild lost connections.
- Hormone optimization: Balancing thyroid, cortisol, and sex hormones improves brain function and reduces further damage.
- Detoxification: We remove harmful toxins like heavy metals and mycotoxins that impede cognitive performance.
- Metabolic improvement: Correcting insulin resistance and mitochondrial dysfunction restores energy production in brain cells.
By tackling these root causes, we help the brain recover. Many post-COVID patients begin noticing improvements in clarity, memory, and energy levels within weeks of starting treatment.
Why Traditional Medicine Can't Solve Post-COVID Cognitive Decline
While traditional medicine typically focuses on managing symptoms with medications, it doesn’t address the underlying causes of cognitive decline. Doctors often prescribe anti-depressants or stimulant medications, but these do not help rebuild brain function or heal the damaged areas. They merely mask symptoms, and without addressing the root causes of the cognitive issues, patients often see only minimal improvement.
The ReCODE Program takes a different approach. By using advanced testing, we identify the factors responsible for cognitive dysfunction, whether it’s inflammation, hormonal imbalances, or metabolic dysfunction. Then, we treat those causes directly, helping the brain restore itself through neuroplasticity-based rehabilitation.
Measurable Recovery Is Possible
Patients following the ReCODE Program show measurable cognitive improvements within 6–9 months. This includes improved memory, faster processing speed, better attention, and restored executive function. In fact, peer-reviewed studies show that over 84% of participants experienced significant cognitive improvements, often reversing mild cognitive impairment (MCI) to normal function.
"The difference with the ReCODE Program is that we don’t just stop decline—we actually reverse it. By addressing the root causes and rebuilding damaged pathways, we give patients back their lives."
— Dr. Garland Glenn
References
- Douaud G. et al. SARS-CoV-2 is associated with changes in brain structure. Nature, 2022.
- Taquet M. et al. 6-month neurological and psychiatric outcomes in COVID-19 survivors. The Lancet, 2022.
- Bredesen DE, et al. Rationale for a Multi-Factorial Approach for the Reversal of Cognitive Decline. Frontiers in Aging Neuroscience, 2023.
- Bredesen DE, et al. Sustained Cognitive Improvement in Alzheimer’s Disease Patients Following a Precision Medicine Protocol. Biomedicines, 2024.
Medically reviewed by Dr. Garland Glenn, DC, PhD, AFMC (Advanced Functional Medicine Clinician)
The Carroll Institute — Sarasota, FL
About Dr. Garland Glenn
For educational purposes only; not a substitute for medical advice.

Dr. Garland Glenn, DC, PhD, IFM, AFMC
Founder & Clinical Director, The Carroll Institute — Sarasota, FL
Dr. Garland Glenn is a board-certified chiropractic physician and functional medicine practitioner specializing in cognitive health, neurodegeneration, and root-cause medicine. Certified as an AFMC (Advanced Functional Medicine Clinician) and Institute for Functional Medicine (IFM) trained, he has also completed over 500 hours of advanced training in Functional Neurology under Dr. Ted Carrick, founder of the Carrick Institute.
At The Carroll Institute, Dr. Glenn leads Sarasota’s only ReCODE-certified Functional Neurology program, helping patients reverse or prevent cognitive decline through the Bredesen ReCODE Protocol, neuroplasticity exercises, and personalized functional medicine care.
Learn more about his background and approach at About Dr. Garland Glenn.
– schedule now –
free discovery call
To help you get started, we offer a free 20-minute Discovery Phone Consultation. During this call, you will be able to talk with one of our Certified Brain Health Coaches about what going on with you or your loved one and find out if we can help. Please review our FAQs prior to scheduling your free call. We look forward to talking with you soon and helping you Save Your Brain.
(yes, it’s totally free!)
ReCODE® is a registered program developed by Dr. Dale Bredesen and licensed through Apollo Health. Dr. Garland Glenn is a certified ReCODE practitioner.